
As CMS continues to see strong results from Chronic Care Management, the calendar year (CY) 2024 Medicare Physician Fee Schedule (PFS) Final Rule did not introduce any significant changes to reimbursement for the program. While the updated conversion factor totaled a 3.37% cut, the slight uptick in RVUs for the CCM coding family largely offset this reduction, resulting in only a minor decrease to reimbursement.
This is especially true for the complex CCM services. CPT 99487, the first 60 minutes of complex CCM services, has the highest reimbursement rate among the CCM coding family. As a result, the $1.22 decrease in reimbursement is relatively small. The reimbursement rate for CCM code 99489 increased by $0.56, indicating a positive development for complex CCM services.
As a significant contributor to the 99487 and 99489 codes, CareHarmony utilizes complex CCM to ensure comprehensive, whole-person care. Only around 55% of CareHarmony’s total CCM codes are contributed to 99490, meaning 45% of our distribution is dedicated to complex CCM and add-on codes for additional time spent with patients. This compares to the industry average of 93% of all CCM code distribution which is attributed to 99490.1
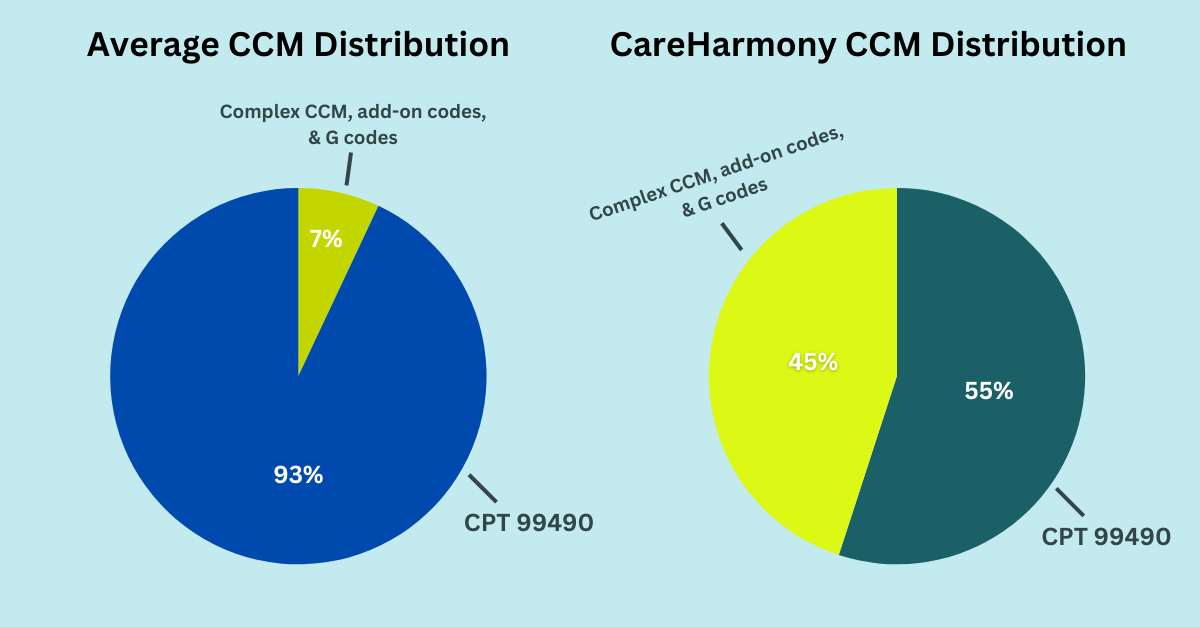
The underutilization of complex CCM codes highlights the difficulty CCM vendors face in demonstrating moderate to complex clinical decision-making, which could be due to many underlying factors including poor patient targeting and the high utilization of Medical Assistants. This can make it difficult to adequately document medical necessity for complex CCM and devote extra time to patients over the 20-minute billing minimum for both regular and complex CCM add-on codes. Similarly, the Social Determinants of Health (now covered under G0511) are often overlooked.
CareHarmony utilizes LPNs and RNs for our services with a focus on comprehensive care plans that integrate the SDoH into clinical decision-making. For context, CareHarmony averages 39-44 minutes per patient per month, with the inclusion of at least one add-on code for 40% of these patients.2 By spending more time with patients, our care coordinators are able to prevent gaps in care and ensure better clinical outcomes.
References
- Use of Chronic Care Management Among Primary Care Clinicians. Ashok Reddy, Leah M. Marcotte, Lingmei Zhou, Stephan D. Fihn and Joshua M. Liao. The Annals of Family Medicine September 2020, 18 (5) 455-457
- CareHarmony Operations Overview Data 2024




